Abstract
Background: DLBCL is the most common histologic subtype of non-Hodgkin lymphoma, accounting for about 33% of all NHL cases. However, the healthcare burden associated with DLBCL has not been extensively studied in a US population. We evaluated the costs of care and healthcare utilization (HCU) of DLBCL patients treated during routine care in the US.
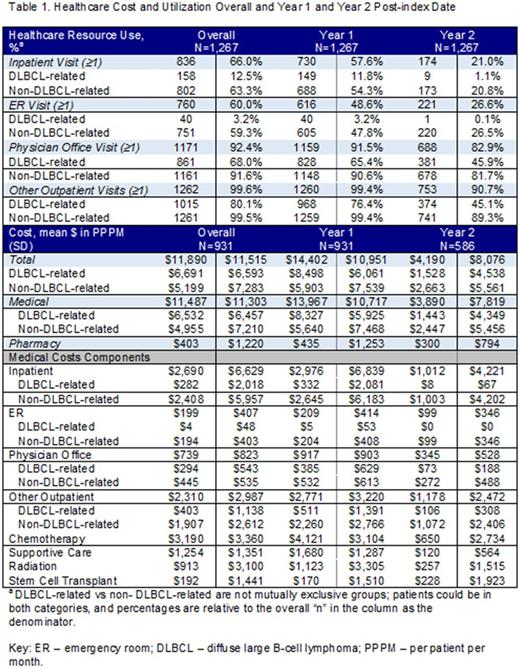
Methods: The Optum claims database was used to identify adult patients (≥18 years old) with newly diagnosed DLBCL between 01/01/08 and 10/31/15. DLBCL diagnosis was based on ≥1 inpatient claim or ≥2 outpatient claims with DLBCL diagnosis codes, with the index date being the first DLBCL claim. Patients were followed from index date until end of continuous enrollment, death, or end of study period (12/31/15) for the assessment of HCU and costs. DLBCL-related and non-DLBCL-related HCU and costs incurred during follow-up were evaluated. DLBCL-related HCU and costs were medical claims with a primary diagnosis of DLBCL or DLBCL-related treatments (chemotherapy, radiation, stem cell transplant (SCT), supportive care) and pharmacy claims for DLBCL treatment. Proportions of patients with HCU were reported. Costs were calculated as per-patient-per-month (PPPM) costs and reported as mean and standard deviation (SD). Patients with a capitated payment plan were excluded from the cost analysis.
Results: 1,267 treated DLBCL patients were identified. Median follow-up from index diagnosis date was 19.5 months (interquartile range: 8.8, 37.3). Over the follow-up period, 66.0% of patients had ≥1 inpatient admission, with more patients having a non-DLBCL-related than DLBCL-related admissions (Table 1). 60.0% of patients had ≥1 emergency room visit over the follow-up period; visits were predominately for non-DLBCL-related. Nearly all patients had ≥1 physician office visits (92.4%) and other outpatient visits (99.6%). The mean PPPM costs incurred during the follow-up period was $11,890 (SD: $11,515) (Table 1), and costs were higher in Year 1 ($14,402, SD: $10,951) than in Year 2 ($4,190, SD: $8,076). About 55% of costs overall were related to DLBCL-medical services ($6,532 PPPM, SD: $6,457). DLBCL-related medical PPPM costs decreased substantially from Year 1 ($8,327, SD: $5,925) to Year 2 ($1,443, SD: $4,349). This decrease was driven by the decreases in chemotherapy and supportive care medical services from Year 1 to Year 2. Non-DLBCL-related medical costs accounted for about 42% of the overall PPPM costs ($4,955, SD: $7,210); and a decrease was observed from Year 1 ($5,640, SD: $7,468) to Year 2 ($2,447, SD: $5,456). Inpatient admission was the main component of non-DLBCL-related costs, and associated costs decreased from Year 1 to 2.
Conclusions: The economic burden associated with the treated DLBCL population is high, with the majority of costs incurred during the first year of diagnosis. Between the first and second year of diagnosis, costs decrease mainly because of the decrease in the DLBCL-related treatment costs. In addition, HCU for DLBCL-related services decreased in Year 1 vs Year 2.
Galaznik: Takeda Pharmaceuticals: Employment, Equity Ownership. Bell: Takeda Pharmaceuticals: Employment, Equity Ownership. Hamilton: Millennium Pharmaceuticals, Inc., a wholly owned subsidiary of Takeda Pharmaceutical Company Limited: Consultancy; Xcenda: Employment. Ogbonnaya: Xcenda: Employment; Millennium Pharmaceuticals, Inc., a wholly owned subsidiary of Takeda Pharmaceutical Company Limited: Consultancy. Hennenfent: Xcenda: Employment; Millennium Pharmaceuticals, Inc., a wholly owned subsidiary of Takeda Pharmaceutical Company Limited: Consultancy. Eaddy: Xcenda: Employment; Millennium Pharmaceuticals, Inc., a wholly owned subsidiary of Takeda Pharmaceutical Company Limited: Consultancy. Shou: Takeda Pharmaceuticals: Employment, Equity Ownership.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal